Isoimmunization, also known as Rh incompatibility, occurs when a pregnant woman’s blood type is incompatible with her baby’s blood type, typically due to the Rh factor. This condition can affect the health of both mother and baby if not managed properly. Understanding isoimmunization, its effects on pregnancy, and how to manage it can help ensure a healthier pregnancy and outcome.
What is Isoimmunization?
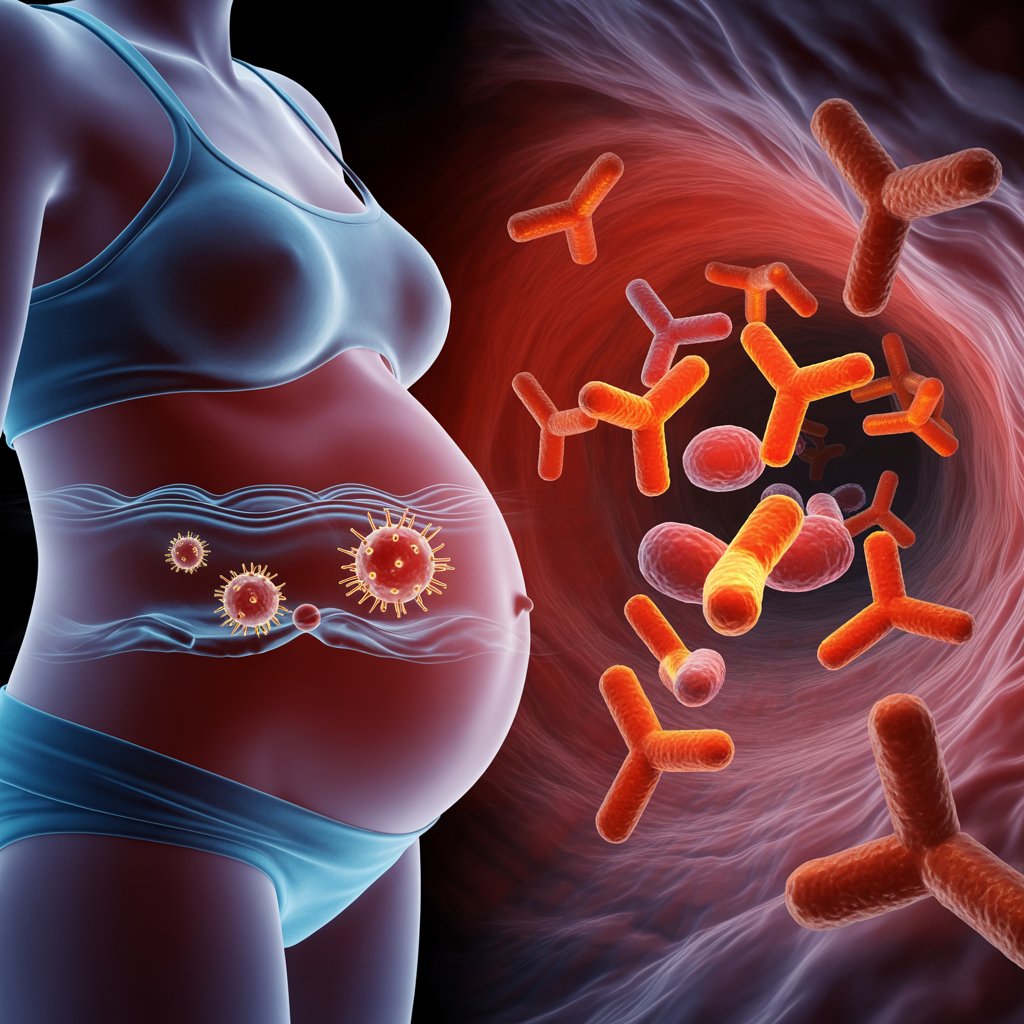
Isoimmunization arises when a Rh-negative mother’s immune system is exposed to Rh-positive blood cells from her baby. This exposure can lead to the production of antibodies against Rh-positive blood. The most common scenario is during childbirth or if there is any bleeding or trauma during pregnancy that allows fetal blood to mix with maternal blood.
If the mother develops these antibodies and becomes pregnant again with an Rh-positive baby, her antibodies can cross the placenta and attack the baby’s red blood cells. This can lead to a condition called hemolytic disease of the newborn (HDN), which can have serious consequences for the baby.
Effects of Isoimmunization on Pregnancy
- Hemolytic Disease of the Newborn (HDN): HDN occurs when maternal antibodies attack the baby’s red blood cells, causing them to break down prematurely. This can lead to anemia, jaundice, and in severe cases, heart failure or brain damage in the baby. HDN can range from mild to life-threatening, depending on the severity of the condition.
- Increased Risk of Preterm Birth: Severe cases of HDN can lead to complications that may necessitate early delivery to protect the baby’s health. Preterm birth carries its own risks, including developmental and respiratory issues for the baby.
- Fetal Growth Restriction: Chronic anemia from HDN can affect the baby’s growth and development, potentially leading to intrauterine growth restriction (IUGR). This means the baby may be smaller than expected for their gestational age.
- Stillbirth: In extreme cases, untreated or severe HDN can lead to stillbirth. However, with proper management and treatment, this risk can be significantly reduced.
Management and Prevention
- Rh Immune Globulin (RhoGAM): The primary preventive measure for isoimmunization is the administration of Rh immune globulin (RhoGAM). This medication is given to Rh-negative women during pregnancy (typically around the 28th week) and within 72 hours after delivery if the baby is Rh-positive. RhoGAM prevents the development of antibodies against Rh-positive blood.
- Monitoring and Testing: Regular monitoring and blood tests are crucial. Your healthcare provider will check for the presence of Rh antibodies in your blood and monitor your baby’s health through ultrasounds and other tests. This helps in early detection of any issues and timely management.
- Treatment of HDN: If your baby develops HDN, treatment options include intrauterine blood transfusions, phototherapy for jaundice, and in severe cases, early delivery. Your healthcare provider will develop a plan tailored to manage the condition effectively.
- Follow-up Care: Regular follow-up care is essential to ensure that any potential issues are addressed promptly. Attend all scheduled prenatal appointments and follow your provider’s recommendations.
Your Role and Next Steps
If you have Rh incompatibility or isoimmunization concerns, working closely with your healthcare provider is key. Ensure you receive RhoGAM injections as recommended and attend all prenatal appointments for monitoring and testing. If you have any questions or concerns about your condition, discuss them with your provider to understand your treatment options and what to expect during your pregnancy. By staying informed and engaged in your prenatal care, you can help manage isoimmunization effectively and contribute to a healthier pregnancy and outcome for you and your baby.

