Monitoring fetal heart patterns is a vital part of prenatal care, offering insights into the well-being of the developing baby. Abnormal fetal heart patterns can indicate potential complications and require careful evaluation to ensure a healthy pregnancy outcome. This educational piece explores common abnormal fetal heart patterns, their potential causes, and approaches to management.
Normal Fetal Heart Rate Patterns
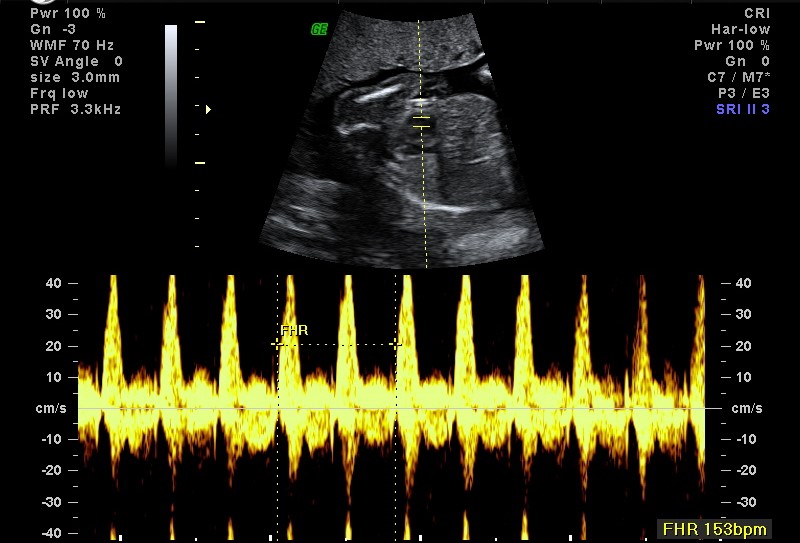
Before delving into abnormalities, it’s important to understand normal fetal heart rates. The typical fetal heart rate ranges from 110 to 160 beats per minute (bpm). Normal variability in the fetal heart rate reflects a well-oxygenated fetus and a healthy autonomic nervous system. Fetal heart patterns are assessed during prenatal visits using techniques like Doppler ultrasound and electronic fetal monitoring (EFM).
Common Abnormal Fetal Heart Patterns
- Tachycardia: Tachycardia is defined as a fetal heart rate above 160 bpm for an extended period. It can result from factors such as maternal fever, dehydration, anemia, or infection. In some cases, it may also be associated with fetal distress or anemia. Management involves addressing the underlying cause, such as treating maternal infection or ensuring adequate hydration, and monitoring the fetal response to interventions.
- Bradycardia: Bradycardia is characterized by a fetal heart rate below 110 bpm. It may indicate a compromised oxygen supply to the fetus, possibly due to umbilical cord compression, placental insufficiency, or fetal arrhythmias. Persistent bradycardia requires immediate evaluation to determine the cause and appropriate intervention, which may include repositioning the mother, administering oxygen, or preparing for an emergency delivery if necessary.
- Decreased Variability: Variability in the fetal heart rate refers to fluctuations in the heart rate from beat to beat. Decreased variability, or minimal variability, can be a sign of fetal distress, often due to hypoxia or medications affecting fetal central nervous system function. It is assessed in conjunction with other indicators, such as contractions and fetal movements. Management may involve additional monitoring and interventions to improve fetal oxygenation.
- Late Decelerations: Late decelerations are characterized by a gradual decrease in the fetal heart rate that begins after a contraction and returns to baseline after the contraction ends. They are typically indicative of uteroplacental insufficiency, where the placenta is not delivering sufficient oxygen to the fetus. Management often includes repositioning the mother, improving hydration, and, in some cases, preparing for an expedited delivery if the condition does not improve.
- Variable Decelerations: Variable decelerations are abrupt decreases in fetal heart rate that vary in duration and timing, usually occurring with uterine contractions. They often result from umbilical cord compression. While they may be benign and transient, persistent or severe variable decelerations may indicate more serious issues. Management includes interventions to relieve cord compression, such as maternal repositioning or amnioinfusion.
Management and Follow-Up
Effective management of abnormal fetal heart patterns depends on accurate diagnosis and understanding of the underlying cause. It often involves a multidisciplinary approach, including obstetricians, midwives, and sometimes neonatologists. Continuous fetal monitoring may be required, along with additional diagnostic tests such as ultrasound or fetal scalp sampling.
Conclusion: Abnormal fetal heart patterns are important indicators of fetal well-being and can signal a range of conditions from benign to severe. Understanding these patterns helps healthcare providers make informed decisions about managing and treating potential issues during pregnancy. Timely intervention and close monitoring are essential to addressing abnormal fetal heart patterns, ultimately ensuring the best possible outcomes for both mother and baby. Pregnant women should feel empowered to discuss any concerns with their healthcare providers, fostering a collaborative approach to prenatal care.

