Cervical shortening is a condition in pregnancy where the cervix, the lower part of the uterus that opens into the vagina, becomes shorter than normal. This can be an indicator of potential complications and requires careful management to ensure a healthy pregnancy. Here’s what you need to know about cervical shortening, including its causes, symptoms, risks, and treatment options.
What Is Cervical Shortening?
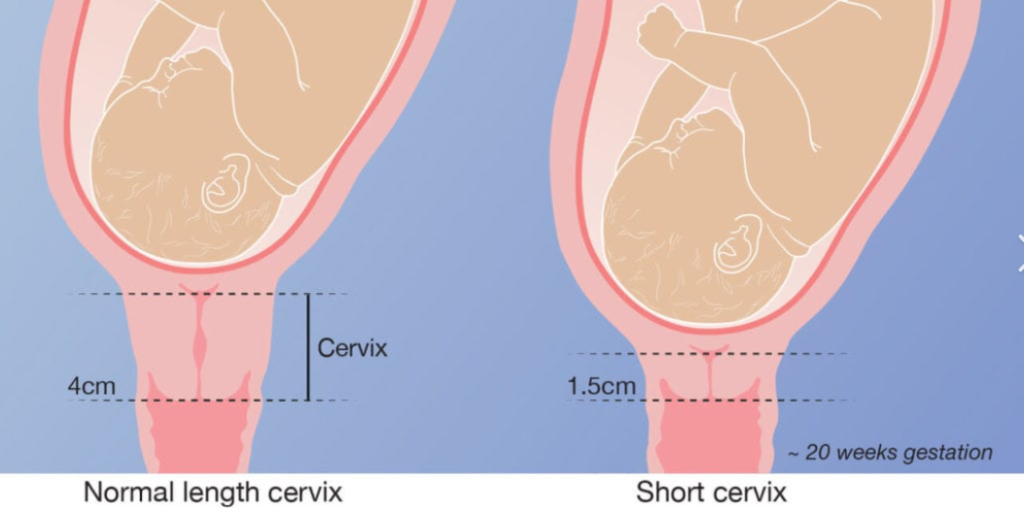
Cervical shortening refers to a reduction in the length of the cervix. Normally, the cervix is long and firm to support the pregnancy. As pregnancy progresses, the cervix naturally starts to soften and shorten in preparation for labor. However, if this process begins too early, it can increase the risk of preterm birth.
Causes of Cervical Shortening
- Inherent Weakness: Some women may have a naturally shorter or weaker cervix due to congenital factors or previous surgeries that affected cervical strength.
- Multiple Pregnancies: Women carrying multiples (twins, triplets, etc.) are at higher risk for cervical shortening due to the increased pressure on the cervix from the larger uterus.
- Previous Cervical Trauma: Previous surgeries or injuries to the cervix, such as a cone biopsy or cervical cerclage, can contribute to cervical shortening.
- Infections: Certain infections can lead to inflammation and shortening of the cervix, impacting its ability to support the pregnancy.
Cervical shortening may not always present with obvious symptoms, but some signs to watch for include:
- Pelvic Pressure: Increased pressure or heaviness in the pelvic area might suggest changes in cervical length.
- Vaginal Discharge: An increase in vaginal discharge, particularly if it is pink or watery, may indicate cervical changes.
- Cramping or Contractions: Early or frequent contractions, particularly if accompanied by pelvic pressure, could signal issues with the cervix.
Diagnosis and Monitoring
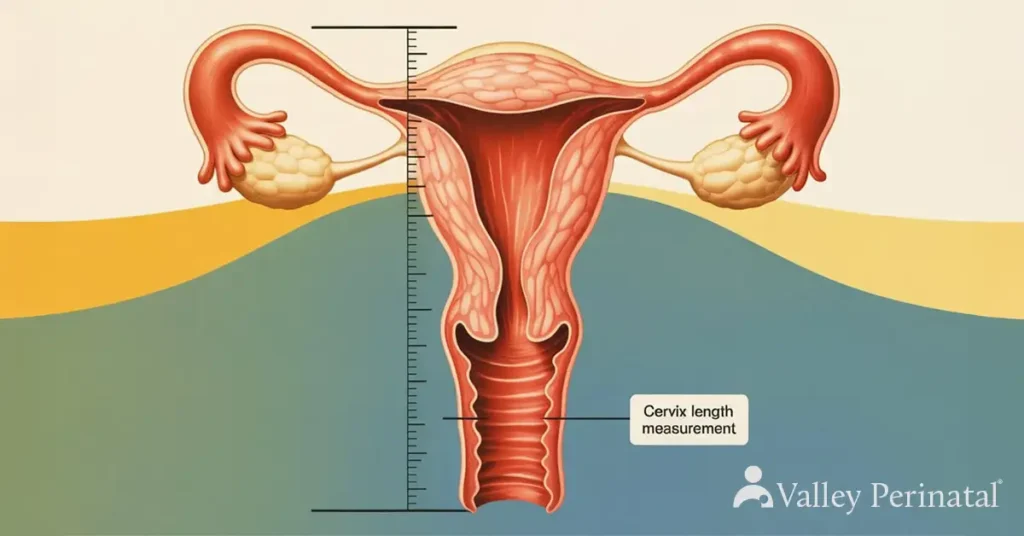
- Ultrasound: A transvaginal ultrasound is the primary method for diagnosing cervical shortening. This imaging technique provides a clear view of the cervix and measures its length accurately.
- Medical History Review: Discussing your medical history, including previous pregnancies or cervical procedures, can help your provider assess risk factors for cervical shortening.
Treatment and Management
- Cervical Cerclage Procedure: A cervical cerclage is a surgical procedure where a stitch is placed around the cervix to provide additional support. This is typically done between 12 and 24 weeks of pregnancy, especially if cervical shortening is detected early. Regular monitoring is necessary to check the cervix’s condition and ensure the cerclage is effective.
- Progesterone Supplement: Progesterone helps maintain the pregnancy and can be prescribed if cervical shortening is suspected or diagnosed. It can be administered through injections or vaginal suppositories to support the pregnancy.
- Rest and Activity: Depending on the severity of cervical shortening, your healthcare provider may recommend reduced physical activity or bed rest to minimize pressure on the cervix.
- Regular Monitoring: Frequent ultrasounds and prenatal visits will be essential to monitor the cervix’s length and manage any potential complications.
Preventive Measures
- Early Prenatal Care: Regular prenatal visits and early detection of cervical changes can help manage risks and intervene promptly if necessary.
- Addressing Risk Factors: If you have known risk factors for cervical shortening, such as a history of cervical surgeries or multiple pregnancies, your healthcare provider can take proactive steps to monitor and manage your condition.
Conclusion: Cervical shortening can pose risks to a pregnancy, but with early detection and appropriate management, many women go on to have healthy pregnancies and deliveries. By understanding the condition, staying informed, and working closely with your healthcare provider, you can effectively manage cervical shortening and support a positive pregnancy outcome. If you have concerns or symptoms suggestive of cervical changes, don’t hesitate to reach out to your healthcare provider for evaluation and guidance.